BY MICHEL CALMON - friday, 10 december 2021
WHAT IS THE GOAL OF THIS BLOGPOST?
To show an innovative response through HAH to overwhelmed hospitals by avoiding the hospitalisation of acute patients in the early phase of COVID (that is, the most risky phase!) and who require continuously oxygen.
The initiative begun from November 2020, i.e., during the 2nd wave of COVID in
France.
The project was launched by Argenteuil Hospital, whose aims were as
follows:
- to avoid overcrowded emergency department,
- freeing
up beds for patients truly in need of hospital beds
- last but not least a more secure and a better quality of life for the patients.
Therefore, Dr Catherine le Gall, head of the
emergency department, came to our HAH Foundation in October and asked us to be able to admit acute patients who
are in the early phase of COVID-19 and require continuous oxygen therapy.
Instead of full hospitalisation
, care in HAH is provided for those patients after being directed by the emergency physicians of Argenteuil Hospital.
WHO ARE THE PLAYERS OF THE INITIATIVE?

The emergency department of one major hospital in the Paris region: the Argenteuil
hospital

And the major player of HAH in France and certainly in Europe: Fondation Santé Service
IN WHAT CONTEXT HAS THE PROJECT OCCURRED?
The 2nd wave in France began in early October.
At that time, there was a debate in the French
medical community on whether we could take care of COVID patients with oxygen at home.
Scientific societies and the HAS (i.e., the National Health Authority) provided on November 9th, what they called quick answers to allow oxygen therapy at home and define the necessary criteria for home care of COVID patients with oxygen therapy.
The quick answer defined 2 kinds of criteria:
1) Environmental criteria:
- fixed and healthy home,
- the presence of a caregiver,
- the patient’s home must be less than 30 minutes from the emergency department
2) And clinical criteria:
- the patient must be autonomous,
- oxygen
requirements must be less than 4 l/min,
- the
02 saturation rate must be more than 92%
WHAT IS THE PATHWAY OF THE PATIENT?
1. The decision to admit was made by the emergency physician based on predefined criteria of the quick answer.
Admission can be decided every day, from 9 am
to 8 pm. After 8 pm, the patient was kept in the emergency room and was included in HAH in the morning.
Therefore, respect
for criteria by the emergency physician
is very important because most of the patients are not seen by the HAH
coordination nurse in the hospital. If the criteria are not respected, the patient must be readmitted to the hospital.
2. Daily monitoring by HAH nurses
Our HAH nursing staff was not numerously sufficient during the second wave, so we decided to work in partnership with independent nurses working close to Argenteuil Hospital. This implies that the coordination had to be still stronger.
The HAH nurse monitors the general state of health, fever, heart rate, respiratory rate, blood pressure, oxygen saturation, diarrhea, discomfort and main risk factors daily.
Then, the HAH nurse can modify the oxygen volume in coordination with the emergency physician.

In case of a deterioration of the state of
health or because of noncompliance with the admission criteria, the emergency
return of patients is organised by the hospital staff. It has always been made
with no problems or objection by the hospital. It was an important point because in this
kind of partnership, trust is essential.
3. Daily and close communication between the emergency department and the HAH nursing staff
This daily communication has been made possible by the use of the regional information system “Terr-eSanté” for exchanges and transmission of information between Argenteuil Hospital and HAH.
Moreover, our coordination nurse had a daily face-to-face meeting with Dr Catherine le Gall, head of the emergency department.
4. Discharge
At the beginning, we planned that the discharge
of HAH was decided by the emergency physician.
However, with the increasing number of patients, we noticed that some emergency
physicians were overwhelmed and that some patients could have been discharged
more quickly. Therefore, emergency and HAH physicians created an
algorithm enabling HAH nurses to decide the discharge of the patient
WHAT ARE THE MAIN FIGURES AND RESULTS?
- Number of admissions per week: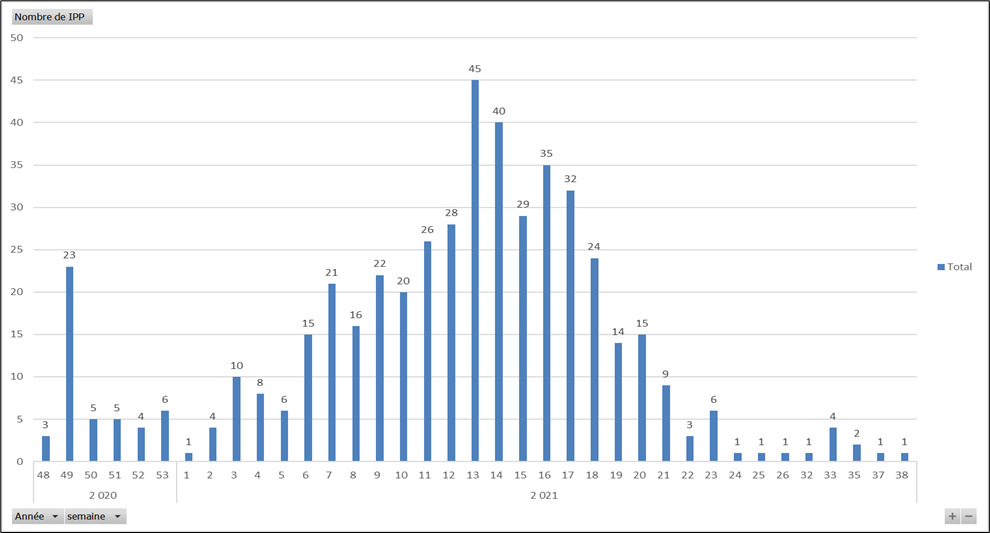
- At the end of September 2021, 463 patients (and 488 stays) were treated in HAH.
- Up to 117 patients were treated per day at the peak of the epidemic in early April (that is to say, as many hospital beds freed up for patients
truly requiring it)
- 35 patients (or 7.1%) were readmitted to hospital
- Average Length of Stay: 18.6 days
- No death at home
- 3 TV reports in national channels (1 report in the main French TV evening
news) and 3 interviews of our HAH doctor in national broadcasts

WHAT ARE THE PROS OF THE PROJECT?
- The
aims of the hospital were largely reached with the decongestion of the emergency room and
finally of the hospital.
- Hospital
at Home had an active and frontline contribution in the management of the
health crisis
- A
low rehospitalisation
rate
When readmission was needed, the emergency department organised it
in complete coordination with HAH.
- Patient
satisfaction
Even though we did not conduct a scientific study, a large
majority of patients expressed satisfaction with having been treated in their home and
surrounded by family and caregivers (whereas in French hospitals during COVID, family was not accepted in the patient’s room)
- The
enhancement of hospital/HAH links
ARE THERE ANY CONS oF THE PROJECT?
- No inclusion of the patient’s own GP and nurse in the pathway
Discharge from the hospital and inclusion in HAH
were too quick to coordinate their role.
- No
interoperability between the regional information system used by the hospital (Terr-eSanté) and the
HAH-one
This implied that the HAH nurses were
compelled to enter both ISs daily, resulting in a major loss of time.
- The
pathway was not designed for such a duration, and such a volume of patients
Several adjustments of the pathway had to be
made for those ten last months, and we faced difficulties in abiding by the pathway during the peak of
the third wave.
TO CONCLUDE, WHAT TAKE AWAY FOR THE FUTURE OF HAH IN FRANCE?
- One major key lesson:
In a French usual pattern, care is prepared upstream at the hospital for a scheduled admission in HAH (48 hours on average). Then, HAH enables a reduction in the length of stay in the hospital. What we learned with this project is that HAH can also avoid hospitalisation on a large scale by treating patients straight from an emergency department.
- The question is: is such a model replicable in a noncrisis context?
We work on it, in two directions:
- focusing
on specific diseases with predefined criteria of admission and more
particularly on geriatric patients.
- Second,
such a model can work only with stronger coordination at every level between the hospital and HAH: doctors
and nurses as well as with IS
Hopefully, we’ll be able to present you soon
the results of the generalisation of HAH care for postemergency patients.
ABOUT THE AUTHOR

Dr Michel Calmon
Fondation Santé Service CEO, French Hospital at Home Federation Vice President and Co-Chair for WHAHC 2021
Publications: Treaty on Medical and Hospital Law (Lexis-Nexis Editions): fascicles on the hospital public service, hospital doctors, hospital organization and management


