To improve quality and safety for the hospital-at-home (HaH), a
foundation for quality improvement is needed that accounts for the unique
nature of home-based acute care while honoring inpatient standards for acute,
inpatient care delivery. Quality
frameworks for the facility-based hospital delivery system have accounted for
such drivers of inpatient quality and safety as timeliness, efficiency, and
patient-centricity. Hospital-at-Home and other forms of home-based care, which
may vary in level of clinical acuity or involve a combination of in-person and
virtual care, require a quality framework that expand on these quality drivers
for the home environment. | | | In 2021, quality and safety leaders from Medically Home Group, Mayo
Clinic and Kaiser Permanente collaborated to devise the Virtual Hospital-at-Home
Quality Framework that honors the nuance of high-acuity hospital-at-home care
that is rapidly scaling with collaboration between virtual and in-home clinicians. We convened expert opinion on quality
standards, while determining a set of core Hospital-at-Home quality indicators,
upon which programs can build quality systems and quality improvement
endeavors. In so doing, we sought
consensus from Hospital-at-Home programs in the United States who have
leveraged virtual care as a core component of care provision to safely scale
home-based care. We elicited feedback
from participating programs in an iterative fashion and aligned our quality
standards to four distinct pillars of the Hospital-at-Home Quality Framework;
each pillar highlights unique areas of importance for our care model as
follows: Differentiating
healthcare access, separate from health equity, demonstrates the unique ability
of HaH care to expand access to acute care, particularly for geographic regions
with limited acute care access. Standards
for expanding access to HaH itself will include expansion of health insurance
reimbursement for HaH care, as well as expansion of points of entry into HaH
programs, inclusive of Emergency Departments, hospital wards, primary care or
urgent care clinics and direct admission from the home. Separately, standards for HaH care will
include equitable care provision that honors patients’ unique differences and
social drivers of health (SDoH); HaH care has an extraordinary capacity for
enhancing equitable care in our health system given its ability to impact SDoH
directly in the home environment.
Safety practices for inpatient hospital settings typically address
the prevention of harm. HaH care demands
this in addition to high reliability of in-home services that are similar to or
better than the traditional hospital along the axes of timeliness, efficiency,
and effectiveness. Highly reliable
in-home services are not only crucial to the delivery of safer care, but are the
primary point of focus for scaling HaH programs that seek to expand acute care
services in a distributed geography. Reliability of in-home service provision
involves such quality standards as identity verification, licensing,
credentialing, service performance and responsiveness, concepts that are
standard for inpatient settings.
Moreover, with distributed teams providing in-home HaH care, Just
Culture and High Reliability Organization (HRO) principles engage HaH providers
in safer, distributed clinical teams and communication patterns. Traditional hospital quality frameworks account for
patient-centeredness; HaH care requires patient- and caregiver- or
family-centeredness. HaH care providers
must be deeply engaged in their clinical care planning to optimize clinical
outcomes. Moreover, the HaH care model
has the potential to reduce provider burnout and improve clinician experience
of care provision, in part because of the unique connection that HaH clinicians
may develop with home-based patients. Provider, caregiver, family, and patient
experience and engagement may be improved in the home, while growth and scale
of the HaH care model requires engagement of providers, patients and caregivers
who have not historically experienced this form of acute care provision. Hospital
at Home is a value-based care intervention, by virtue of improving quality of
care while reducing total cost of care for the healthcare delivery system. The value equation (value=quality/cost) may
be applied to the above quality pillars, with the goal of improving value by
increasing the numerator while maintaining or reducing the denominator. To scale HaH programs, services must be
provided safely and economically in a way that improves value for patients in
need of acute care. The support of government,
health insurance and public health stakeholders in HaH care will depend upon
the value that HaH care provides to patients and families. | | | 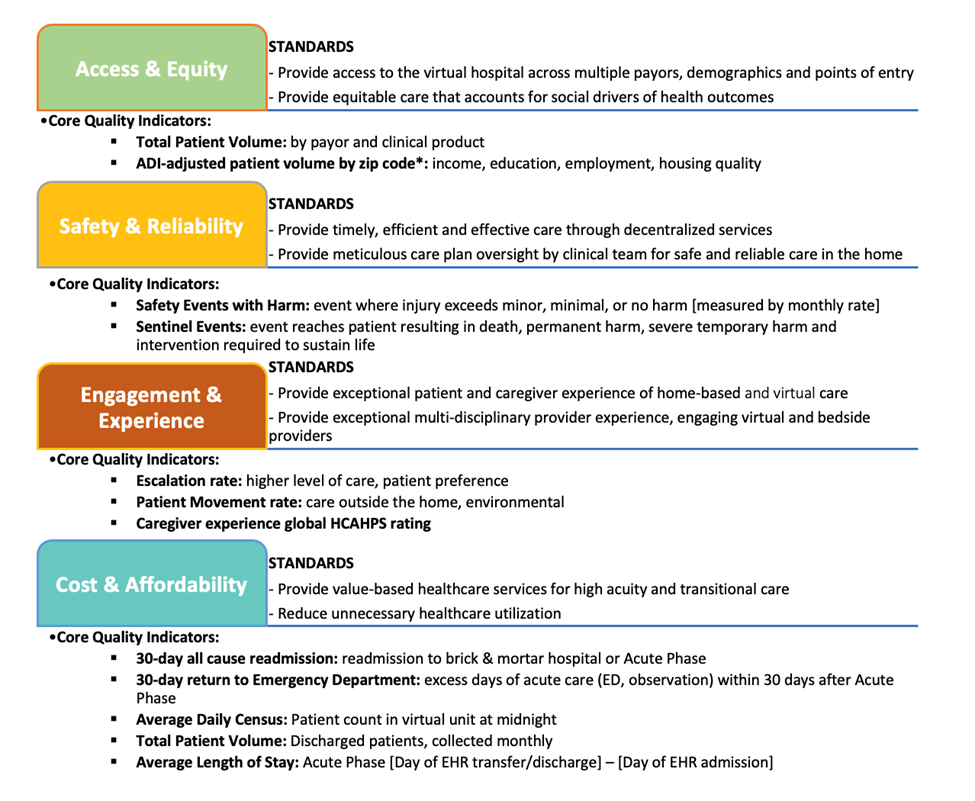
Click here to view the whole poster
| | | Conclusion
By distilling and highlighting these principles, quality leaders
from Medically Home Group, Mayo Clinic, and Kaiser Permanente defined core HaH
quality indicators for the purpose of benchmarking against the standards
associated with each pillar of the Virtual Hospital-at-Home Quality
Framework. In this way, the Virtual HaH
Quality Framework serves as a foundation for quality improvement endeavors, as
well as a foundation for the addition of novel standards and indicators to advance
HaH quality and safety in practice. Further
Research
Future
directions for the HaH Quality Framework are underway and will include further
specification of such quality indicators as 30-day mortality, rate of discharge
to post-acute facilities, and demographic variables of patients served in HaH
programs. Risk adjustment of quality
indicators and establishment of standardized data definitions will facilitate
benchmarking between HaH programs, to enhance quality across all HaH programs
by further defining best practice. | | | ABOUT THE AUTHOR | | |  Gregory Snyder
Gregory Snyder is a clinician and physician innovator applying technology and novel care model design to improve healthcare quality. He is a graduate of the Sidney Kimmel Medical College at Thomas Jefferson University, Brigham & Women’s Hospital Internal Medicine, and Harvard Business School. He practices hospital medicine within the Mass General Brigham system at Newton-Wellesley Hospital and is an Entrepreneur-in-Residence at the Mass General Healthcare Transformation Lab. Greg is a Clinical Assistant Professor at Tufts University School of Medicine and is Associate Faculty at Ariadne Labs. He is focused on designing, co-operating and scaling virtual care and home hospital programs as Vice President, Clinical Strategy & Quality Improvement for Medically Home. He is Medical Director for Primary Care at Piction Health, an AI-guided diagnostic assistant. | | | Co-authors: Gregory D Snyder (1), MD, MBA, Jed Colt Cowdell (2), MD,
MBA, Hemali Sudhalkar (3), MD, MPH, SFHM, Vasiliki Patsiogiannis (1), MPH, CPH, Ellen
Love, MHA (2), Joeffrey R Hatton (3), MBA, Pippa Shulman (1), DO, MPH
- Medically Home Group Inc., 500 Harrison Ave, Boston,
MA, 02116,
- Mayo Clinic, Jacksonville, FL, 32224,
- Permanente Medicine, Oakland, CA, 94612
| | |
|